We treat a variety of wounds and our approach is driven by latest research developments with tried and proven methods.
What Is A Leg Ulcer?
A leg ulcer is simply a break in the skin of the leg, which allows air and bacteria to enter the underlying tissue. This is usually caused by an injury, often a minor one causing the breach in the skin. In most people, such an injury will heal up without difficulty within a week or so. However, when there is an underlying problem, particularly with the circulation, the skin does not heal and the area of breakdown can increase in size and remain open. This is a chronic leg ulcer. Up to 10% of the population over the age of 70 years have a leg ulcer.
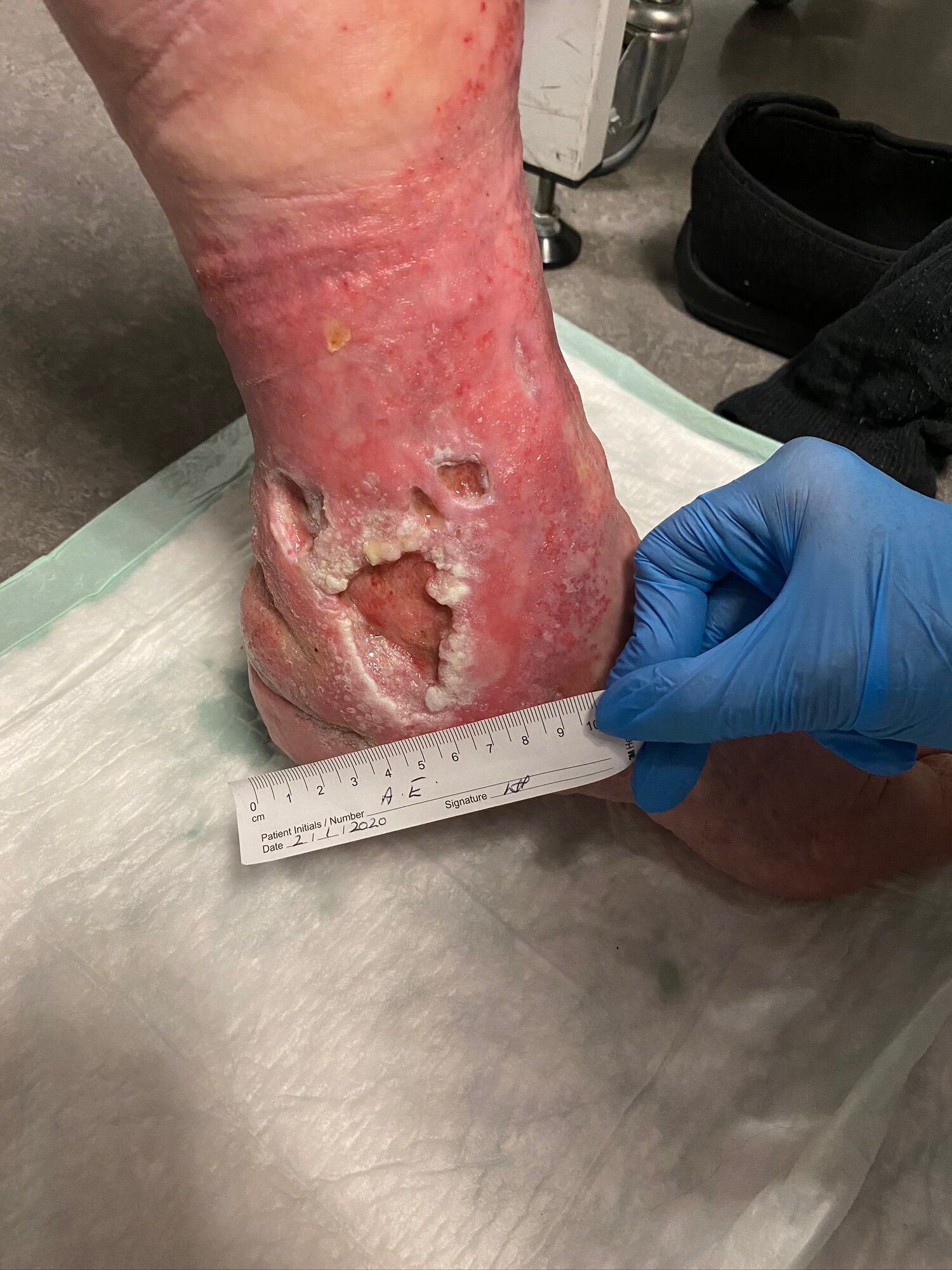
Venous Ulcers
Venous leg ulcers affect around one to three per 1,000 of the UK population, and represent about 80% of all leg ulcers. Most cases are seen in older people and an estimated 2% of people over the age of 80 have a chronic venous leg ulcer. Veins are blood vessels that passively carry blood from the foot and leg back to the heart. These leg veins have valves enabling the blood to flow upwards. Sometimes, these valves don’t work or are impaired by previous thrombosis or blood clot. When the valves are damaged, blood flows back down the veins, resulting in abnormally high pressure in the veins. This high pressure in the veins leads to damage of the skin. Eventually the damage to the skin can leads to the ulcer formation. Venous leg ulcers are often painless but can become painful, especially when infected. If untreated, venous ulcers can gradually increase in size.


Arterial Ulcers
Arterial ulcers, also known as ‘ischaemic ulcers’, are caused by an insufficient blood supply to the lower extremities. This is also known as ‘peripheral vascular disease’. It is often caused by risk factors such as high blood pressure, diabetes, smoking and high cholesterol. They are more common in males and the elderly. The skin and tissues of the feet and ankles are deprived of oxygen and so the overlying tissues die off causing the area to form an open wound – an ulcer. In addition, the insufficient blood supply means that even minor cuts and scrapes can fail to heal and often develop into ulcers. Arterial ulcers are usually painful and can cause pain at night time. Left untreated, arterial ulcers can lead to very serious complications, including tissue death and gangrene needing, extreme cases, amputation of toes and even the lower leg.
Diabetic Foot Ulcers
Diabetes affects more than three million people in the UK and about 15% of diabetic patients suffer with diabetic foot ulcers. This is because in diabetes, abnormal blood sugar levels over time damages nerves in the lower leg, leading to a lack of sensation to the foot. This nerve damage coupled with a restricted or poor blood flow into the foot (also as result of the diabetes) allows ulcers to develop more commonly than in the rest of the population. Diabetes often slows down the healing process of wounds and ulcers and makes them more susceptible to infection. Unfortunately, due to the impaired healing process, diabetic foot ulcers remain a chronic health problem in many patients and profoundly affects their quality of life.


Pressure Wounds
A pressure ulcer is damage to the skin and the deeper layer of tissue under the skin. This happens when constant pressure is applied to the area, usually a pressure point such as over the buttocks or heel, cutting off or restricting the blood supply. Lying in bed or sitting in a chair for long periods of time predisposes to pressure ulcers, also referred to as ‘bed sores’ or ‘pressure sores’. They affect between one to five in every 100 people who are admitted to hospital. If not treated, pressure ulcers tend to become infected and cause damage to the underlying tissues. They also take a long time to heal.
Surgical Wounds
A surgical wound is a wound associated with an incision after an operation. The wound can have problems in the days or weeks following surgery. Sometimes wounds will not heal even though the surgery itself is successful. Chronic infection, even a low-grade infection, delays healing. This is particularly so after bowel surgery, or surgery around the back passage/buttock area. After surgery, there is also a condition known as ‘hypergranulation’ or ‘over-granulation’. This is where there is an overgrowth of healing or ‘granulation’ tissue and the overlying skin fails to grow. The granulation tissue sits ‘proud’ of the surrounding skin. This issue can become a chronic problem and this necessitates specialist wound healing techniques. We also treat wounds after plastic surgical procedures where the incisions have not healed as planned. We are treating an increased number of post-plastic surgery issues at The Wound Clinic.


Accident-Related Wounds
Wounds caused by trauma, accidents, or bites, including insect, animal, and even human bites, can carry a high risk of infection and may heal slowly without proper care. Sports injuries, especially from water sports and contact activities, often require specialist wound management to ensure safe and effective recovery. We also frequently treat patients who return to the UK with wounds sustained abroad, often complicated by unusual infections that need expert attention. At The Wound Clinic, we provide tailored wound care solutions for accident-related injuries, helping patients recover quickly and safely with personalised treatment plans.
Cosmetic Surgery Wounds; UK and Abroad
Many patients experience wound complications after cosmetic surgery, whether performed in the UK or abroad in countries such as Turkey or South America. Procedures like breast reconstruction, tummy tucks, and mummy makeovers can sometimes lead to painful, slow-healing wounds that are both physically and emotionally challenging. Sadly, some patients feel judged or unsupported when seeking help through the NHS or other clinics, leaving them unsure of where to turn. At The Wound Clinic, we offer a welcoming, non-judgmental environment where patients receive expert wound care tailored to their individual needs. We have successfully treated a wide range of cosmetic surgery-related wounds, helping patients heal safely, comfortably, and with renewed confidence.
Cancer-Related Wounds
Many patients living with cancer develop painful and distressing wounds that significantly affect comfort and quality of life. These may result from radiotherapy, infected indwelling venous catheters, or tumour-related skin breakdown, including complex breast wounds that can be large, painful, and malodorous.
Such wounds require highly specialised care delivered with great gentleness and sensitivity. At The Wound Clinic, we have extensive experience in managing a wide range of cancer-related wounds, with a focus on expert treatment, symptom relief, and preserving dignity.
Pressure Wounds in Patients with Paraplegia and Tetraplegia
At The Wound Clinic, we frequently care for patients with paraplegia or tetraplegia who are living with pressure wounds. These complex wounds are often difficult to manage, and many patients do not have access to the ongoing specialist care or long-term support they need within the NHS. We have successfully treated many pressure wounds, either by seeing patients in our clinic or by providing care in the comfort of their own home through home visits.
Wounds In Children
Fortunately, chronic wounds and ulcers are far less common in children than in adults. When they do occur, they are often associated with long-standing conditions such as inflammatory bowel disease or cancer, and require highly sensitive, meticulous wound care.
More commonly, children present with wounds related to trauma, leaving parents understandably anxious and unsure where to turn. Children experience and cope with illness very differently from adults, and this must always be carefully considered. At The Wound Clinic, we have specialist experience in caring for children with wounds, providing expert treatment delivered with compassion, reassurance, and a child-centred approach.